On this page
What Is a Thoracic Aortic Aneurysm?
The aorta — the largest artery in the body — carries all the blood that is pumped out of the heart. Thoracic aortic aneurysms are bulging, weakened areas in the wall of the aorta. They occur in the part of the aorta that runs from the aortic arch to the diaphragm, and the diaphragm to the abdomen.
How common are thoracic aortic aneurysms?
Approximately 15,000 Americans are diagnosed with thoracic aneurysms (TAA) each year. Thoracoabdominal aortic aneurysms (TAAA) are less common.
What are the types of thoracic aortic aneurysms?
There are two types of thoracic aortic aneurysms:
- Descending thoracic aortic aneurysm – A descending thoracic aortic aneurysm occurs in the part of the aorta that runs downward through the chest (thorax).
- Thoracoabdominal aortic aneurysm – A thoracoabdominal aortic aneurysm is one that is located in the area where the aorta crosses between the chest and abdomen.
What causes thoracic aortic aneurysms?
Aortic aneurysms occur because of tissue changes in the wall of the aorta. These changes sometimes cause the aorta to narrow or become blocked due to conditions like atherosclerosis, which causes plaque to build up inside the arteries. This can cause a breakdown of the muscular layer in the aorta, resulting in aneurysms.
Traumatic injury and aortic dissection are other conditions that can cause thoracic aortic aneurysm.
What are thoracic aortic aneurysm risk factors and complications?
Thoracic aortic aneurysm risk factors
Risk factors for thoracic aortic aneurysms include:
Complications of thoracic aortic aneurysm
TAAs and TAAAs are serious health risks because they can burst or rupture, causing severe internal bleeding that can rapidly lead to shock or death.
How serious is a thoracic aortic aneurysm?
The larger the aneurysm, or the faster it grows, the more likely it is to rupture.
The risk of rupture increases when the aneurysm is larger than about twice the normal diameter of a healthy aorta.
How can I prevent thoracic aortic aneurysm?
You may not be able to control some of your aortic aneurysm risk factors. However, preventing heart disease and chronic conditions can reduce the risk that you will develop an aortic aneurysm. You may be able to reduce your risk of developing aortic aneurysm by:
- Avoiding smoking.
- Eating a diet that is rich in fruits, vegetables, and whole grains.
- Exercising and maintaining a healthy weight.
- Limiting alcoholic beverages.
- Maintaining normal blood pressure and cholesterol levels.
Back to top
What Are the Signs and Symptoms of a Thoracic Aortic Aneurysm?
Descending thoracic aortic aneurysms (TAAs) and thoracoabdominal aortic aneurysms (TAAAs) often go unnoticed, yet early diagnosis is critical to managing these conditions.
Only half of people with TAAs and TAAAs have symptoms, which may include:
- Back pain.
- Jaw pain.
- Shortness of breath.
When should I see a doctor about my thoracic aortic aneurysm symptoms?
Aortic aneurysms can cause life-threatening bleeding if they rupture. If you experience symptoms of an aortic rupture, you should dial 911.
Back to top
How Do You Diagnose a Thoracic Aortic Aneurysm?
If your doctor suspects a TAA or TAAA, you'll need to undergo a thorough physical exam and evaluation.
What to expect during your visit
To diagnose a thoracic aortic aneurysm, your vascular surgeon will:
- Ask about your symptoms.
- Discuss your medical history.
- Perform a thorough physical exam.
Tests to diagnose thoracic aortic aneurysm
Following your exam, your doctor may order additional tests and procedures to help confirm the presence and size of the thoracic aneurysm. These diagnostic tests may include:
- Chest x-ray – A chest x-ray is a diagnostic test that uses invisible electromagnetic energy beams to produce images of internal tissues, bones, and organs onto film. An x-ray can show enlargement in any area of the heart.
- Ultrasound – This painless test uses sound waves to create images of your arteries. It also enables your doctor to measure blood flow through your arteries
- Echocardiogram (ECHO) – This noninvasive ultrasound test uses sound waves to evaluate your heart's chambers and valves. The ECHO sound waves create an image on a monitor as an ultrasound transducer is passed over your heart.
- CT scan – A CT scan is a test that creates images of your heart.
- MRI scans – MRI is a diagnostic procedure that uses a combination of large magnets, radio frequencies, and a computer to produce detailed images of organs and structures within your body.
- CT angiogram – A CT angiogram is an imaging test that examines the blood vessels that supply your heart muscle. It uses a powerful X-ray machine to produce images of your heart and heart vessels.
Thoracic aortic aneurysm prognosis
Your prognosis after diagnosis with a thoracic aortic aneurysm depends on the size and extent of your aneurysm. Aortic aneurysm rupture, for example, is a serious, life-threatening condition with a low survival rate. However, if your aneurysm has not ruptured, your doctor may be able to provide surgical treatment that reduces the risk of aortic rupture.
Back to top
How Do You Treat a Thoracic Aortic Aneurysm?
UPMC offers a full range of state-of-the-art aneurysm treatment options for TAAs and TAAAs. Aneurysm treatment depends on its size and location and your overall health.
Monitoring
If your aneurysm is small and does not cause symptoms, your doctor may recommend monitoring your condition. Surgeons consider aneurysm repair surgery when the TAA or TAAA becomes large.
How fast does a thoracic aortic aneurysm grow?
Thoracic aortic aneurysms grow at different rates depending on the size of the aneurysm and where it is located. Because the risk of rupture increases as your aneurysm grows, your doctor will monitor your aneurysm closely to reduce your risk of rupture.
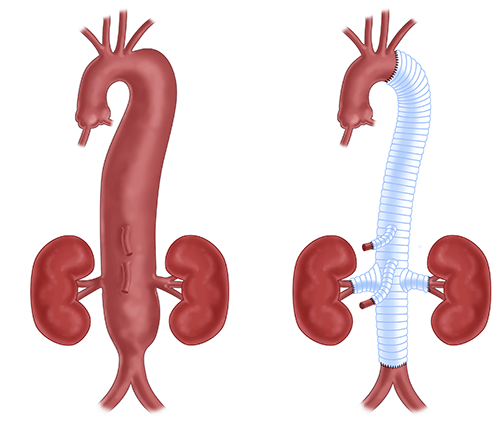
Open aneurysm repair surgery
If your aneurysm is six centimeters in diameter or more, your doctor may recommend surgery. During open thoracic aortic aneurysm repair, your surgeon will:
- Make an incision in your chest.
- Repair or bypass vessels if the aneurysm involves important branches of the aorta.
- Replace the weakened portion of the aorta with a fabric tube called a graft.
After surgery, you will stay in the hospital for 5-7 days. Most patients make a complete recovery in 2-3 months, depending on the complexity of your surgery, your overall health, and whether you have other conditions such as heart, lung, or kidney disease.
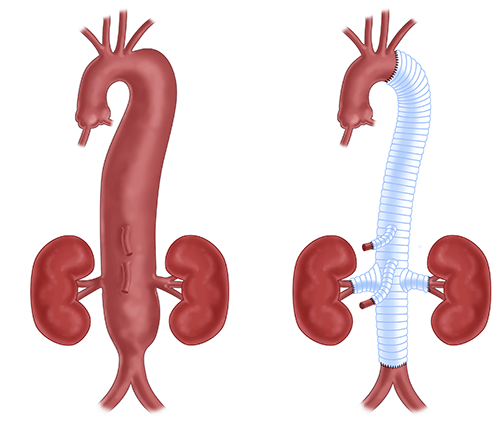
Endovascular aneurysm repair (EVAR)
Your surgeon may recommend repairing your thoracic aortic aneurysms with a minimally invasive EVAR procedure. Whether or not you can have EVAR procedure depends on the shape, location, and extent of the aneurysm.
In contrast to a traditional “open" surgery, no big incisions are made in the chest. Instead, the arteries in the groin are accessed either by a needle puncture or a small incision.
During EVAR, your doctor will:
- Insert a small, thin tube called a catheter through a small incision into a blood vessel in your groin.
- Use the catheter to guide a small metal and fabric tube called a stent through your blood vessels to the aneurysm.
- Expand the stent so it holds the weakened portion of the aorta open, redirecting blood flow through the stent to relieve pressure on the bulging aorta.
After an EVAR, most people recover quickly and can often go home the next day. However, because the stent can shift over time, yearly follow-ups with your surgeon are required.
EVAR reduces your hospital stay by 2-3 days and requires less recovery time when compared to traditional open thoracic aortic aneurysm repair.
If EVAR is not an option for you, you may have access to other minimally invasive treatment options. UPMC routinely participates in clinical trials of leading-edge devices to treat complex aortic aneurysms.
How effective is treatment?
Many open aneurysm repairs are successful in the long term with few complications. Follow-up after open aneurysm repair is less frequent than that for EVAR, with most patients coming back every 2-3 years for a checkup.
However, EVAR requires more frequent follow-up visits and imaging studies to ensure that the graft continues to function properly. You also may require periodic maintenance procedures.
What is the life expectancy of someone with a thoracic aortic aneurysm?
Your life expectancy depends on whether you receive early, effective treatment, the size and extent of your aneurysm, and whether your aneurysm has ruptured. Your doctor will discuss your life expectancy with you.
Back to top
Why Choose UPMC for Thoracic Aortic Aneurysm Care?
At UPMC, you have immediate access to state-of-the-art diagnostic and treatment options for thoracic aortic aneurysm. When you choose UPMC, you will benefit from:
- Our advanced imaging technology – Sophisticated 3D imaging technology allows our surgeons to plan advanced treatment options for the thoracic and thoracoabdominal aorta.
- Our minimally invasive care – We offer minimally invasive endovascular thoracic aortic repair with stent grafts for aortic aneurysms, dissections, and traumatic injuries.
- Our valve-preserving techniques – If necessary, our surgeons can perform complex aortic valve repair procedures.
By UPMC Editorial Staff. Last reviewed on 2024-10-01.